Coplegia is a medical word that can sound strange and scary. Many people see or hear it by accident and wonder what it really means. While it is not a word most doctors use every day, coplegia links closely to a group of serious movement problems that affect the muscles and nerves. When we break it down into simple language, coplegia usually refers to a form of paralysis that affects more than one part of the body.
In this article, we explain coplegia in clear terms. We explore its definition, main symptoms, common causes, and how health professionals look for it and help treat it. Our goal is to help you understand what coplegia may describe, what signs to watch for, and what steps to take if you or someone close to you shows paralysis or severe weakness.
Coplegia Explained: What Does the Term Mean?
The word coplegia does not appear in every textbook, but it is built from two Greek roots often used in medicine: “co” for together, and “plegia” for paralysis. So, coplegia usually points to paralysis that affects two or more limbs or parts of the body at the same time.
In practice, when people search for coplegia, they are often looking for information about kinds of paralysis such as:
- Hemiplegia paralysis on one side of the body, such as the right arm and right leg
- Paraplegia paralysis of both legs and often the lower body
- Quadriplegia or tetraplegia paralysis of all four limbs
- Diplegia paralysis that mainly affects the same area on both sides, like both legs
When we use the word coplegia in this guide, we are talking about serious weakness or loss of movement that affects more than one body part at the same time. It is a sign that something has gone wrong in the nervous system, usually in the brain, spinal cord, or the nerves that control the muscles.
How Coplegia Affects the Body
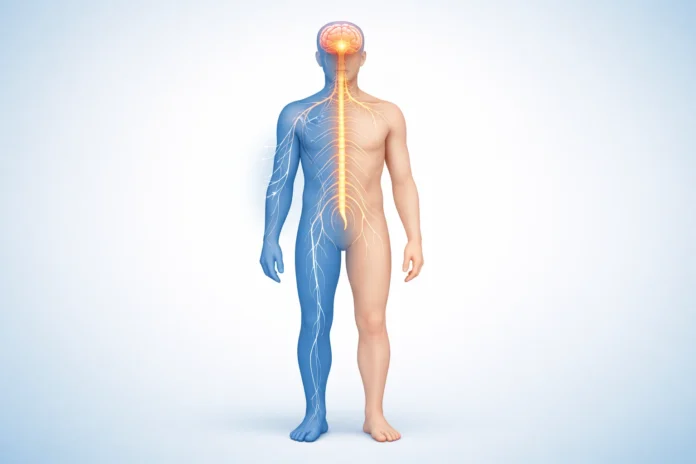
Coplegia changes the way signals travel from the brain to the muscles. Under normal conditions, your brain sends tiny electrical messages down the spinal cord, out through the nerves, and into your muscles. These messages tell the muscles when and how to move.
When part of this system is damaged, the messages do not get through clearly or at all. This can lead to weakness or full loss of movement in more than one limb or region. The effect depends on where the damage happens.
For example, damage high in the spinal cord may affect both arms and both legs. Damage in one side of the brain may mainly affect the opposite side of the body. When such changes show up in pairs of limbs or in large body areas, doctors may describe the condition in terms similar to coplegia.
Main Symptoms of Coplegia
The symptoms linked to coplegia can range from mild weakness to complete loss of movement. They may appear suddenly, such as after a stroke or accident, or they may develop slowly over months or years, as in some nerve diseases.
Loss of Voluntary Movement
The most important sign of coplegia is loss of control over muscles in more than one limb. A person may not be able to:
- Lift or move an arm or leg on command
- Stand, walk, or balance without help
- Grip objects tightly or move fingers with purpose
In severe coplegia, the affected limbs may not move at all, even when the person uses all their effort to try.
Muscle Weakness and Fatigue
Before full paralysis, many people notice heavy weakness in both legs or both arms. Simple actions like climbing stairs, lifting a cup, or getting out of bed become hard. The muscles may feel tired very quickly, even with small tasks.
Changes in Muscle Tone
Coplegia often comes with changes in the way muscles feel when touched or moved:
Some people develop stiff, tight muscles. Their joints resist movement, and their limbs may lock in bent or straight positions. Others develop floppy, soft muscles that offer little resistance to movement. The type of change often gives clues about the location and type of nerve damage.
Abnormal Reflexes
Doctors will usually check reflexes with a small hammer or simple tests. In some forms of coplegia, reflexes become very brisk or overactive. In others, they become weak or absent. These patterns help identify the level of the nervous system affected.
Loss of Sensation or Strange Feelings
While coplegia mainly describes movement problems, sensation can also change. Some people notice numbness, pins and needles, burning pain, or loss of feeling in the same areas that are weak or paralyzed. These sensory changes can be just as troubling as the loss of strength.
Problems with Balance and Coordination
Because coplegia may affect both sides of the body, many people struggle to stay upright or steady. They may fall easily, drag one or both legs, or feel like their body does not respond quickly enough to keep balance.
Common Causes of Coplegia
Coplegia is not a disease by itself. It is more like a signal that something has harmed the nervous system. The causes are wide and varied. Some appear suddenly and are medical emergencies. Others develop slowly and require careful testing and long term care.
Stroke
Stroke is one of the most common causes of sudden paralysis that may match what people call coplegia. A stroke happens when blood flow to part of the brain stops or when a blood vessel bursts. Brain cells start to die within minutes.
When the stroke affects movement areas, a person may suddenly lose strength in one side of the body or in both legs. Fast medical care during the first few hours can sometimes limit damage and improve recovery.
Spinal Cord Injury
Trauma to the spine from car crashes, falls, sports injuries, or violence can damage the spinal cord. Since the spinal cord carries nerve messages between the brain and the body, damage often causes coplegia-type paralysis below the level of injury.
For example:
- An injury in the neck may cause weakness or paralysis in both arms and both legs.
- An injury in the mid or lower back may affect both legs but spare the arms.
Swelling around the spinal cord can make paralysis worse in the early days, so quick treatment is vital.
Traumatic Brain Injury
A severe hit to the head from an accident, fall, or sports contact can harm the brain. If the areas that control muscles are injured on both sides, the result can be coplegia-type symptoms. Some people go into a coma first and wake up to find that parts of their body no longer move as before.
Neurological Diseases
Several diseases that affect nerves or the protective myelin around them can lead to weakness or paralysis in multiple limbs. These include:
- Multiple sclerosis (MS)
- Guillain Barre syndrome
- Motor neuron disease such as ALS
- Chronic inflammatory demyelinating polyneuropathy
In these conditions, symptoms usually build over time. A person may first feel tingling or mild weakness, then gradual loss of power spreading to both sides of the body. In the later stages, coplegia level paralysis may appear.
Infections Involving the Nervous System
Some infections can attack the brain, spinal cord, or nerves directly. Examples include:
- Meningitis or encephalitis
- Polio or polio like viral infections
- Spinal abscess or severe local infections near the spinal cord
These infections can cause sudden or subacute weakness. When both legs or more than one region is affected, the pattern may match what people describe as coplegia.
Autoimmune and Inflammatory Conditions
In autoimmune diseases, the immune system mistakenly attacks the body’s own tissues. When this attack targets the nervous system, coplegia like problems may follow. Conditions such as neuromyelitis optica or some forms of vasculitis can inflame the spinal cord or brain and rapidly lead to multi limb paralysis.
Tumors and Compression
Growths in or near the brain and spinal cord can slowly press on nerves and tissue. As pressure builds, muscle weakness and sensory loss may spread to both sides of the body. A spinal tumor, for example, may quietly grow until it compresses the cord enough to cause coplegia type paraplegia.
Metabolic and Toxic Causes
Certain toxins, drugs, and metabolic imbalances can interrupt nerve signals. Heavy metals, some chemotherapy medicines, and severe lack of vitamins such as B12 can damage nerves. In rare cases, this damage can become so wide that it leads to major weakness on both sides of the body, similar to coplegia.
How Doctors Diagnose Coplegia Related Conditions
Because coplegia itself is more a description than a diagnosis, the most important job for doctors is to find the cause behind the paralysis. This process usually includes several steps.
Medical History
The first step is a careful talk with the patient, family, or witnesses. Doctors ask when the weakness started, how fast it grew, and what other symptoms came with it. They also ask about recent injuries, infections, travel, medicines, and other health conditions.
Neurological Examination
The physical exam helps map out how coplegia affects the body. A doctor will check:
- Muscle strength in all limbs
- Reflexes with a hammer
- Muscle tone and posture
- Balance, walking pattern, and coordination
- Touch, pain, vibration, and temperature sense
The pattern of findings often points to whether the trouble is in the brain, spinal cord, or peripheral nerves.
Imaging Tests
Magnetic resonance imaging (MRI) or computed tomography (CT) scans help show detailed pictures of the brain and spinal cord. These tests can reveal stroke, bleeding, tumors, swelling, infections, or traumatic injury that might explain coplegia.
Blood Tests and Other Studies
Blood work can look for infections, autoimmune markers, vitamin levels, toxins, or metabolic problems. In some cases, doctors may perform a lumbar puncture to examine the fluid around the brain and spinal cord.
Nerve conduction studies and electromyography (EMG) may also be used to measure how well nerves and muscles carry signals.
Treatment Options for Coplegia Related Paralysis
Because coplegia is the result of many possible conditions, treatment always focuses first on the root cause. At the same time, care teams work to protect remaining function, prevent complications, and support recovery.
Emergency Care
When coplegia appears suddenly, emergency care may save life and function. For example:
- Stroke treatments aim to restore blood flow or control bleeding.
- Acute spinal cord injuries may need surgery to stabilize and decompress the cord.
- Severe infections call for strong antibiotics or antiviral medicines.
In these moments, rapid action within hours can make a real difference in long term strength and independence.
Medications
Depending on the cause, doctors may use:
- Anti inflammatory or immune suppressing drugs for autoimmune conditions
- Antibiotics, antivirals, or antifungals for infections
- Blood thinners or clot busting drugs in some stroke cases
- Muscle relaxants to help with stiffness and spasms
- Pain relievers for nerve and muscle pain
These medicines do not cure coplegia by name, but they help fight what is causing the paralysis and ease symptoms.
Rehabilitation and Physical Therapy
Rehabilitation is one of the most important parts of life after coplegia related insults. Physical therapists, occupational therapists, and sometimes speech therapists work together to help the person regain as much function as possible.
Therapy may include:
- Exercises to strengthen muscles that still work
- Stretching to reduce stiffness and prevent joint contractures
- Training in wheelchair use, transfers, and safe movement
- Practice with daily tasks such as dressing, bathing, and eating
Even when full recovery is not possible, small gains in strength, skill, and confidence can bring big changes in daily life.
Assistive Devices and Adaptive Tools
People living with long term coplegia often benefit from equipment tailored to their needs. This may include wheelchairs, braces, walkers, grab bars, modified utensils, or technology that helps them control devices with limited movement.
These tools give more independence and reduce the strain on family members and caregivers.
Mental and Emotional Support
Coplegia and paralysis can be emotionally heavy. People may grieve the loss of movement, feel anger, shame, or sadness, or worry about their future. Families also face stress as they adjust to new care roles.
Counseling, support groups, and open conversations with loved ones can help. Mental health care is not a luxury in this situation, but a key part of healing. Many people find strength and new meaning even after serious disability, especially when they feel heard, supported, and included in decisions.
Living With Coplegia: Practical Tips for Daily Life
Life with coplegia asks for patience, planning, and teamwork. While every person’s path is different, some general steps can help:
- Keep regular follow ups with your neurologist or rehabilitation doctor.
- Ask for a home safety check to reduce fall risks and ease movement.
- Learn skin care to prevent pressure sores from long sitting or lying.
- Watch for signs of urinary infections, breathing trouble, or blood clots, and seek care early.
- Set small, realistic goals for progress and celebrate each step forward.
Over time, many people and families become experts in managing their own version of coplegia. They find new ways to work, study, enjoy hobbies, and take part in community life.
When To Seek Medical Help For Possible Coplegia
Any sudden loss of strength, feeling, or movement in more than one limb is an emergency. Call 911 or your local emergency number if:
- You cannot move an arm or leg suddenly.
- Weakness spreads quickly to both sides of the body.
- Weakness comes with trouble speaking, seeing, or thinking clearly.
- You have loss of bladder or bowel control with back pain or numbness in the groin area.
For gradual changes, such as slowly increasing weakness, numbness, or falling more often, schedule a prompt visit with your doctor. Early testing can catch serious conditions before damage becomes permanent.
Key Takeaways About Coplegia
Coplegia is a term closely linked to multi limb paralysis and severe weakness. Though it is not a standard everyday label, it reflects a real group of conditions that affect the brain, spinal cord, and nerves. The main message is simple: coplegia like symptoms are always serious and deserve careful medical attention.
By knowing the main signs, causes, and treatment options, we can respond faster, ask better questions, and support those who live with these challenges. With expert care, steady rehabilitation, and strong emotional support, many people with coplegia related paralysis find ways to build a meaningful life with new routines, skills, and hopes.
Frequently Asked Questions About Coplegia
What is coplegia in simple words?
Coplegia, in simple words, refers to paralysis or very strong weakness that affects more than one part of the body, such as both legs or an arm and a leg. It is not a disease by itself but a sign that something has damaged the nervous system.
Is coplegia the same as quadriplegia?
Quadriplegia means paralysis of all four limbs. Coplegia is a broader word people sometimes use online to talk about multi limb paralysis. Quadriplegia is a specific medical term, while coplegia is more general and less standard.
Can coplegia be cured?
Whether coplegia can improve or not depends on its cause. Some people recover a lot of strength after stroke, infection, or certain nerve problems, especially with early treatment and strong rehab. Others may have permanent paralysis, such as from severe spinal cord injury. In these cases, care focuses on adaptation, prevention of complications, and quality of life.
What are early warning signs that may lead to coplegia?
Early signs can include tingling or numbness in both feet or hands, weakness that spreads to both sides of the body, trouble walking or frequent falls, and sudden loss of strength after an injury or stroke like event. Any of these should prompt a medical check.
How is coplegia different from simple muscle weakness?
Simple muscle weakness, such as after flu or lack of exercise, is usually mild, affects the whole body evenly, and improves with rest. Coplegia type weakness is stronger, often affects specific limbs or sides in a clear pattern, and is tied to nerve or brain damage rather than simple tired muscles.
Can children develop coplegia type paralysis?
Yes, children can develop forms of paralysis that resemble coplegia. Causes include birth injuries, infections, spinal cord trauma, certain genetic or autoimmune diseases, and conditions like cerebral palsy. Early diagnosis and therapy are very important to support growth and development.
Which doctor should I see if I suspect coplegia?
If symptoms are sudden or severe, go to the emergency room right away. For slower changes, start with your primary care doctor, who will likely refer you to a neurologist. In many cases, a team that includes a neurologist, rehabilitation doctor, and therapists will work together to manage coplegia related problems.